General medicine case -9
This is an online e log book to discuss our patient de-identified health data shared after taking his /her /guardians signed informed consent.Here we discuss our individual patients problem through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input.
This e blog also reflects my patients centered online learning portfolio and your valuable inputs on the comment box is welcome.
A 38 years old male patient ,cooking by occupation ,from miryalaguda came to OPD on 16.11.2021 with the complaint of fever since 5 days and burning micturation since 5 days , abdominal pain since 4 days.
History of present illness :-
-Patient was apparently asymptomatic 3 yrs back ,then he went to hospital with complaint of increase in frequency of urination.
-There he came to know that he was diabetic then he was prescribed oral hypogycemic drugs .
-1month back on routine checkup he came to know that his blood sugar levels was more than normal .(>300)
-Patient daily wake up 7 o'clock in the morning fresh up and by 10 am he went to his work .
- Before starting of abdominal pain ,he was feeling slight weakness from 2 days .
- He used to take mostly idli ,chapathi ,little amount of rice from the day of abdominal pain . (Lower abdomen at umblicus region) .
-He went to hospital at miryalaguda ,there he was suggested to our hospital .
-Fever which is intermittent type ,more during night time .
-Frequency of urination is more of which he was unable to control and he sometimes passes urine in his clothes .
-He also has pain in the loin region .
-Frequent urination with burning sensation
- Patient also has a habit of stoppage of urine at working place.
-He was diagnosed with hypertension after admitted in our OPD .
History of past illness :-
-History of diabetes since 3 yrs .
-No history of hypertension ,asthma, epilepsy , previous surgery.
Personal history :-
-Diet :- mixed .
-Appetite :- normal
- Bowel and bladder movements :- Increase in frequency of urination .
-Sleep :- Normal
Family history :-
- No history of similar complaints in family members .
Drug history :-
- No history of allergy to known drugs .
General examination :-
-Patient is conscious, coherent, cooperative and well oriented to surroundings .
-No history of cyanosis, clubbing, lymphadenopathy, pallor .
Vitals :-
Temperature :- 100 °F
Pulse rate :- 86 beats /min
Respiratory rate :- 20 cycles /min
Blood pressure :- 150/100 mmHg
SPO2 :- 98%
GRBS:- 274 mg %
Systemic examination :-
-CVS :- S1,S2 +, no murmurs heard
-Respiratory system :- Bilateral air entry is normal .
- Abdomen :- Tenderness at the lower abdomen region .
- CNS :- Patient is conscious, coherent, cooperative and well oriented to surroundings. Speech is normal .
Investigations :-
Fever chart
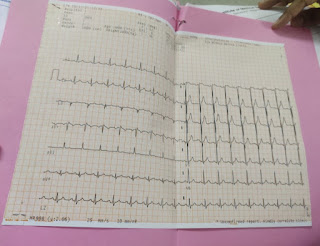
ECG:-
Diagnosis :- Acute pyelonephritis
Treatment :-
1) Inj .FALCIGO 120 mg IV OD
2) Inj .MEROPENUM 1gm IV TID
3)Inj. NEONOL 100ml IV TID
4)Tablet Liprofloxacin 500 mg PO BD
5)Tablet Doxy 100mg PO OD
6) Tablet PCM 1000mg PO
7) Tablet Pan 40mg PO OD
8) Tablet Amlong 5mg PO OD
9) Tablet Urisdas 1mg PO OD
10) Inj. HUMAN INSULIN S/C TID


















Comments
Post a Comment